Nick TriggleHealth Correspondent
 Getty Images
Getty ImagesThe number of flu patients in England's hospitals has risen by more than 50% in the past week, with NHS chiefs warning there is no sign of a “super flu” peak yet.
In the week to Sunday there were an average of 2,660 flu cases a day in hospitals and NHS England said the numbers had continued to rise this week.
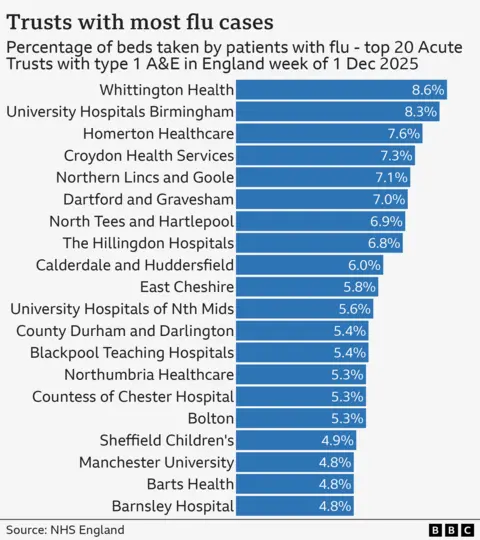
NHS England said this is the equivalent of having three hospitals full of flu patients, with some reporting nearly one in 10 beds are occupied by patients with the virus.
Officials said the number had continued to rise this week, with fears it could top 5,000 by the weekend. Increases have also been reported in other parts of the UK.
Children and young people aged five to 14 had the highest rates of flu in England.
But in terms of who suffers or gets sick most, flu hospitalization rates in England are highest among people over 75 and children under five.
NHS England medical director Professor Meghana Pandit said: “This unprecedented wave of superflu leaves the NHS facing a worst-case scenario for this time of year – with staff stretched to the limit to continue to provide the best possible care to patients.”
The number of flu hospital admissions at this time of year is at its highest level since records began – although they only date back to 2021 and so do not reflect the two worst flu seasons of the last 15 years, seen in 2014-15 and 2017-18.
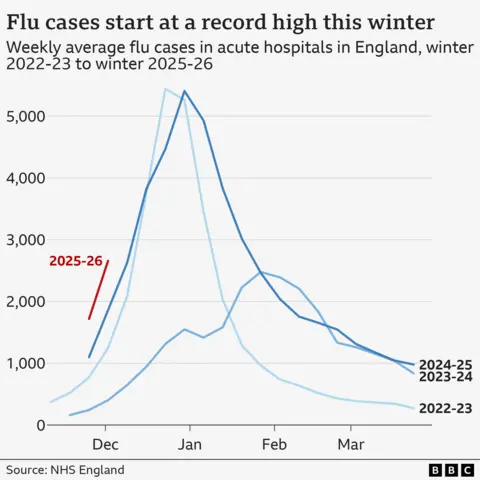
This year, flu cases began to rise a month earlier than usual due to a mutated strain of the virus. The dominant strain is H3N2, but it has undergone some genetic changes this year.
This means that the general public has not been exposed to this exact version of the flu before, meaning there may be less immunity.
NHS England said the number of patients in hospital with the vomiting-causing norovirus is also rising, with more than 350 beds occupied by people with the virus.
It comes ahead of a strike by resident doctors (the new name for junior doctors) due to begin next week.
There are hopes it could be called off after a new proposal from Health Secretary Wes Streeting prompted the British Medical Association to agree to poll its members to see if they would be willing to call off the five-day strike due to start on Wednesday. The results of this vote will be announced on Monday.
Prime Minister Sir Keir Starmer accused the BMA of being “irresponsible” and said he should accept the proposal, adding that the proposal could only be implemented if they ended the strike, “especially in the run-up to Christmas, especially when we have a flu problem.”
Daniel Elkeles, from NHS Providers, which represents hospitals, said: “The NHS is in the midst of a storm that is coming early. The flu has hit hard, and other winter infections are on the rise.
“Now more than ever, the NHS needs all hands on deck.
“We must hope that BMA resident doctors will abandon their strike action next week, accept the government’s reasonable offer and end the damaging dispute.”
Buckling system
Data from the UK Health Security Agency (UKHSA), which looks at infection rates in the community as well as in hospitals, shows infection rates continue to rise, but not as sharply as the previous week.
However, officials stressed that it is too early to take this as a sign that the flu may be peaking.
They said the virus is unpredictable and a lull may be followed by a new surge.
Dr Conall Watson, UKHSA infectious diseases expert, urged people who are eligible for a free flu vaccine from the NHS, including people over 65, people with certain health conditions and pregnant women, to still come forward if they have not yet received it.
“There is still enough flu vaccine available to protect those who need it, but time is running out for protection before Christmas.
“If you're eligible, this is your last chance to get protection before Christmas, so book an appointment with the NHS today.”
Dr Watson says it can take up to two weeks after vaccination to ensure maximum protection from the jab.
Dr Vicky Price, president of the Society of Emergency Medicine, said winter viruses were putting additional strain on an “already fragile system”.
She said patients were facing long waits in emergency departments because hospital staff were overwhelmed with patients.
But she accused NHS England and the government of using her as a “convenient scapegoat” for the “predictable breakdown” in NHS capacity caused by workforce shortages.
“The situation in emergency departments has become so dire that what was once considered a critical incident is now seen as normal and routine. What is happening is not an isolated emergency, but the culmination of a systemic failure.”