Anne Marie Hukriede appealed her insurance company's decision not to cover her daughter's scoliosis surgery three times.
The answer was the same each time: Aetna considers the procedure doctors recommend for her 12-year-old daughter Vivian to be experimental, citing a lack of evidence of its long-term safety and effectiveness.
When the third denial came on November 11, this time from an outside independent medical expert who reviewed the case on Aetna's behalf, Vivian's surgery was just days away. Considering the procedure could cost up to $100,000 out of pocket, the family put it off.
Hukride, who lives in Centennial, Colorado, exhausted her last chance to appeal last month. Now Vivian's ideal window to access treatment is closing, as the surgery must be done while the baby is still old enough. (Girls' peak growth spurts typically occur between ages 10 and 14.)
“It’s disheartening and disappointing,” Hukride said. “You're angry. We pay a lot of money in insurance premiums to keep everything covered.”
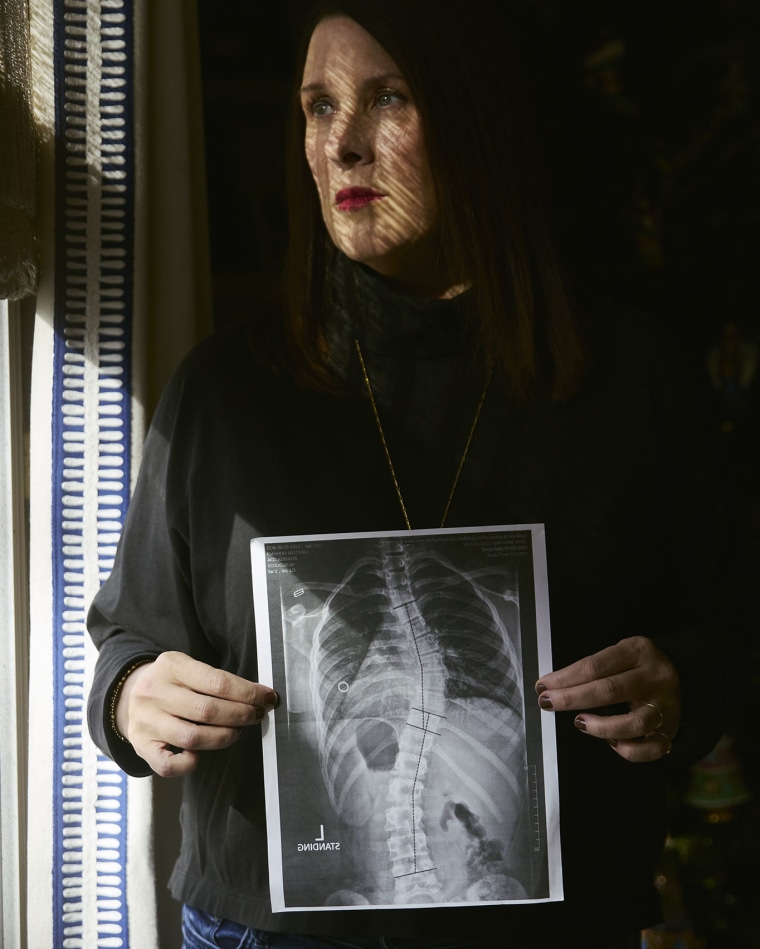
Scoliosis is an abnormal curvature of the spine that is most often diagnosed in adolescents. Around 3 million cases are diagnosed every year. While most are mild and cause no symptoms, moderate to severe cases can lead to back pain, breathing problems and limited mobility. For Vivian, whose spine curves like a question mark, the condition makes it painful for her to sit in school or attend dance competitions, her favorite pastime.
“There are a lot of things that are not easy for me to do because of my back,” Vivian said. “I really want to keep dancing and I think dancing will be a lot easier after the surgery.”
Vivian's dance competition season was set to begin in January, and the Houkriedes sued Aetna on Monday, asking a Colorado district court to force the company to reverse its refusal.
In a statement, Aetna said it is “committed to supporting physicians in making decisions about the care of their patients based on the best available medical evidence, including peer-reviewed research and regularly updated clinical guidelines.”
The company did not respond to NBC News' inquiry about the lawsuit.

The procedure Vivian's doctor recommended, called vertebral body tethering (VBT), involves attaching a flexible cord, known as a “tether,” made by the medical device company Highridge, to the vertebrae along a curved section of the spine. As the child grows, the harness straightens the curve, slowing the growth of one side of the spine and promoting growth of the other.
Food and Drug Administration approved Tether in 2019 for children with worsening scoliosis, determining that “The likely benefits outweigh the possible risks.” Many doctors recommend it for teenagers whose spine is still growing, which means there is still time to correct the curvature. Scoliosis Research Society and Pediatric Orthopedic Society of North America jointly recommend insurance companies cover the surgery. But like Aetna, many other insurers still consider it too experimental.
In Vivian's case, Aetna said a panel of clinical experts “concluded that VBT was beyond the standard of care for a 12-year-old child with scoliosis.” The company added that “evidence shows that VBT procedures have higher complication rates and poorer outcomes compared with standard posterior spinal fusion for scoliosis.”
The standard fusion procedure cited by the company uses rods and screws to stiffen the spine. But the rods can restrict people's movement and injure healthy discs, potentially leading to back pain or the need for additional surgeries later on. Using the cable, patients can maintain range of motion without the risk of disc degeneration, surgeons say. Either option requires a hospital stay of approximately two to three days, and subsequent recovery may be shorter due to tethering.
The main risk with a harness is that since it is flexible, it will break over time. Surgeons estimate that about 20% of patients will require spinal fusion or subsequent spinal replacement surgery.
Four surgeons who were not involved in Vivian's case but also perform vertebral body fixation rejected Aetna's characterization of the surgery's risks and outcomes, saying the benefits have become more apparent over time as surgeons learn which patients are best suited.
“It's a sad day for me when I see someone who really is the indicated, ideal candidate for a procedure, and I can't provide that,” said Dr. Daniel Hornschemeyer, a pediatric orthopedist at the University of Missouri Health Sciences who is a paid speaker at Highridge and is on its medical education team.
Several surgeons said denials like Aetna's are an example of how insurers have been slow to change their coverage policies to include the latest medical innovations. Some reported spending hours each week arguing with insurance companies over tethering denials.








